The deadline for the largest-ever grant funding programme for medication management closes in under 151 days. Now is the time to apply or check that your plan passes the Connected Medication Management test to maximise grant benefits of up to $22,000 per site.
It was not surprising to learn that using a rudimentary paper system to manage the medications of residents with complex requirements did not minimise medication errors. The surprise is how long it’s taken to be addressed. Given that medication errors caused the highest number of complaints to the Royal Commission and significant unplanned hospital visits, fixing this problem has been one of the highest priorities in the Governments plan.
Medication problems
High rates of polypharmacy in residents are a source of medication errors in aged care. More than 37%1 of Australian aged care residents are on polypharmacy, i.e. they are taking nine or more prescription medications, and over 20% are taking antipsychotic medications. Having separate unconnected records for the facility, pharmacist and doctor also leads to errors. A review2 found 72.6 errors in the records per 100 medications, with 48% able to cause moderate harm and 9.8% severe harm. These are unacceptable and unnecessary risks.
Significant time is also lost trying to confirm data or relay new information as the pharmacists and doctors are not under the same roof. One study3 revealed that facilities send 7 faxes or calls per shift to pharmacists or GPs, 30 minutes completing forms and another 30 minutes transferring the data into clinical care systems. This is time that could be better spent directly providing care.
Software benefits
The benefits of medication management software have been hiding in plain sight. Hospital studies 4 show 58% fewer medication error rates as unclear, illegible and incomplete orders are wiped out and serious clinical errors fall by 44%. These are stunning results and contrary to the usual drip feed of headlines reporting IT system delays or non-delivery.
It’s important to note these benefits occur in an environment where the doctor and pharmacist are under the same roof making coordination easier if not guaranteed. Transplanting a hospital-style medication management platform is not enough, given the complexities in aged care facilities, which is why you need to look at the back of the box to see what the medication management software does.
Connected Medication Management
To gain the grant funding, your medication management vendor must comply with the new eNRMC standard (electronic National Residential Medication Chart). This will provide one digital medication record with access to the latest resident data. However, minimising medication errors needs more than just abandoning paper and adopting eNRMC compliant software. It’s vital to have Connected Medication Management software to address the consumer’s complexity.
Connected Medication Management works by enabling seamless two-way communication, so all the care team is informed about the latest medication changes, sharing observations and/or consumer reactions. This is in addition to the GP, Pharmacy and Facility accessing the same live medication chart. It also allows the pharmacy to directly send medication data to their packing systems avoiding re-transcribing that can introduce medication errors.
4R Test
To check if your software provides Connected Medication Management, ask about the 4R’s. Is the RELEVANT information available in REAL time in the RIGHT place – so the whole care team can view records in real-time – and without RE-TRANSCRIBING? Only Connected Medication Management systems pass all these tests to maximise patient safety. Many vendors will point to their system being connected because the information can be sent to the pharmacy by electronic messaging. In practice, this is ineffective as it often requires re-transcribing at the pharmacy, opening the door for avoidable medication errors.
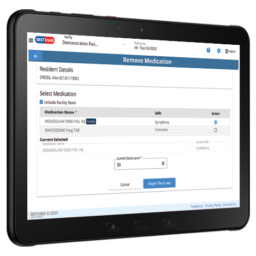
BESTMED
Finally, it’s vital to select a vendor with a long-term commitment to medication management quality and avoid those not making continuous improvements. BESTMED invests $2.5m pa in research and development to eradicate medication errors and is already working on next-generation solutions in partnership with Macquarie University5 researchers. It’s why over 500 facilities and 50% of the largest providers choose BESTMED’s Connected Medication Management for their consumers.
2. The General Practice and Residential Aged Care Facility Concordance of Medication (GRACEMED) study
3. Examining the role of information exchange in residential aged care work practices – a survey of residential aged care facilities.
4. Effects of two commercial electronic prescribing systems on prescribing error rates in hospital in-patients: a before and after study
5. https://www.mq.edu.au/research/research-centres-groups-and-facilities/healthy-people/centres/australian-institute-of-health-innovation/news-and-events/news/news/new-grant-will-transform-medication-safety-in-aged-care
First published in Aged Health, 27 October 2022
Click here for more information about the eNRMC and government grant opportunity funding now available.
ENQUIRE NOW
If you would like a demonstration of the BESTMED electronic Medication Management system, please contact Amir Sinanovic on 0427 685340 or click below to email.